An introduction to the different kinds of maternity care and choosing the best care for you.
“Public or Private?”
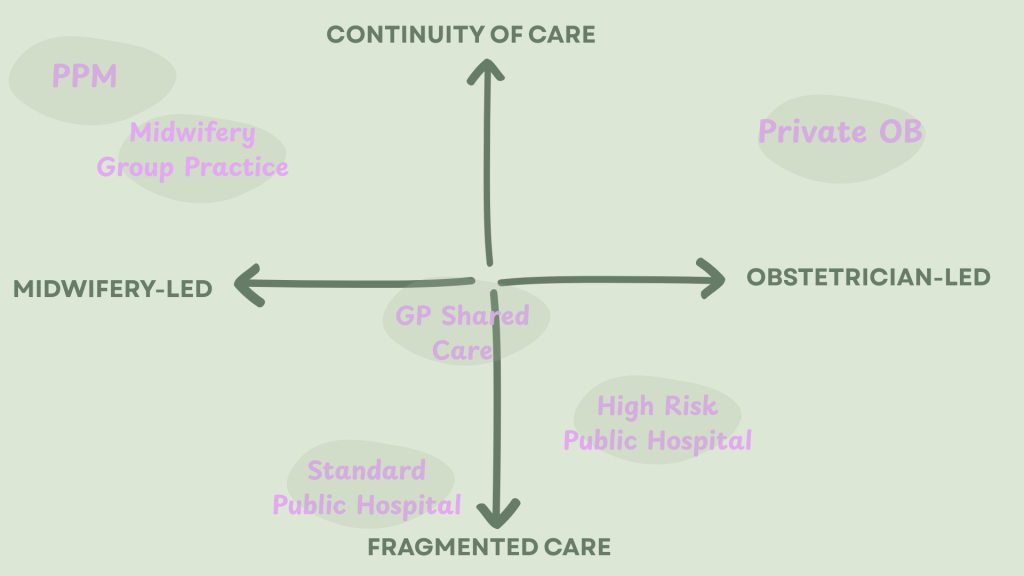
That’s one of the first questions the GP asks when you fall pregnant. It implies that, here in Perth, we only have two choices for clinical care during pregnancy, birth and postpartum: The first is fragmented midwifery care in the public system. The second is continuity of care led by a private obstetrician- if you can afford it, that is!
In my first pregnancy, I also believed that there really were just two choices. But that’s not actually true!
In terms of medical support, there are different types of providers, as well as different models of care, and they are not mutually exclusive of each other.

This topic is close to my heart because, after my first baby, my eyes were opened to all the models of care that are out there- even the ones that “they” don’t tell you about.
This knowledge was what ultimately led to the most amazing and empowering birth and postpartum experience with my second baby.
So let’s explore the options!
OBs and Midwives- what is the difference?
The following is the job description for an Obstetrician (OB), according to the Australian Government’s Jobs and Skills website:
“Obstetrician and Gynaecologists provide diagnostic, treatment and preventative medical and surgical services related to the care of women, foetuses and children during pregnancy and childbirth, and to disorders of the female genital, urinary, rectal and reproductive organs.”

In other words, an OB’s role is to manage complications, disease and injury. That’s pretty damned important, thank goodness we have OBs!
However, it’s not actually their role to care for women in the general course of their pregnancy, birth and postpartum. According to Jobs and Skills, that is the role of a midwife:
“Midwives provide care and advice to women during pregnancy, labour and childbirth, and postnatal care for women and babies in a range of settings such as the home, community, hospitals, clinics and health units.”
That’s a completely different job!
Different Care Providers = Different Care Philosophies
With such different modes of operation, these care providers would, naturally, develop different philosophies regarding the nature of birth (whether it is safe or dangerous) and the role of medical intervention.

During my first pregnancy, I was under the care of a private OB. He was lovely, but he pathologised my extremely normal (boring, even!) pregnancy, and recommended totally unnecessary interventions. When looking at the above descriptions, it seems I should have expected that that was going to happen, because I chose the wrong care provider for me.

One of my heroes, Dr Melanie Jackson, has said that hiring a private obstetrician in an uncomplicated pregnancy is a bit like hiring a paediatrician to babysit your kids.
I love that! I wish I had heard it before my first baby. She also talks about aligning your personal birth philosophy with that of your care provider. That was advice I took right into my second pregnancy.
The second time around, I enlisted the care of a privately practising midwife (PPM). Her philosophy was that birth works, most of the time. She did exactly what the midwives are meant to do, and supported my health and wellbeing during my pregnancy, birth and postpartum journey. This care was so thorough and holistic, fostering both physical and mental wellness, giving me the best possible start to my second motherhood era. In so doing, she gave my baby the possible start too.
The Different Models of Care: Your first decision in pregnancy
Some models of care are considered to be “continuity of carer” or “caseload” models, where the woman is with a known provider throughout pregnancy, birth and postpartum. The opposite of this is sometimes referred to as “standard care” or “fragmented care”. And, naturally, there are some care models that are somewhere in the middle.
Continuity of Care Models
Continuity of care models include:
- Private obstetric care
- Private midwifery care
- Publically funded midwifery programs, such as Community Midwifery Programs (CMP) or Midwifery Group Practice (MGP) available at certain hospitals, and through birth centers.
- Partially funded offerings from other organisations, such as Western Obstetrics here in Perth.
Where do they operate?
Private obstetricians conduct most antenatal and postnatal care in their offices, and birth is done in hospitals.

Privately practicing midwives (PPMs) will usually conduct antenatal and postnatal appointments in the woman’s home.
For birth, most PPMs have admitting rights at one or more hospitals.
The women in their care often choose homebirth, but some would prefer to birth in a hospital, or require access to hospital services such as caesarean section.
In these cases, the women still get the continuity in the antenatal and postnatal time, plus their chosen midwife can attend their birth in hospital in a clinical role.
CMP and MGP vary from program to program, and midwives may attend births at home, in a birthing center or in hospital. Again, there will be guidelines that determine which women are eligible for each of these options.
The Bad News
Unfortunately, these programs are inaccessible to around 70% of women.
Engaging a private obstetrician or a privately practicing midwife incurs a large out-of-pocket expense, which sadly puts them out of reach for many.

Whilst CMP & MGP programs are publicly funded, they usually have very strict guidelines for who is eligible, which again makes it difficult for most women to access them. I, myself, was “risked-out” of using these programs, due to medical history that ultimately does not impact on birth.
Plus, if you are one of the 7 million Australians who live rurally/regionally, this will further limit your options.
If you have the luxury of choice, you are in the minority
The Standard Care Model
The most common model of care in Perth is midwifery care though the public hospital system. This model, whilst being completely funded by the government, offers no continuity of care to women, and they may see a different midwife at every appointment, during birth and postpartum.

Sometimes care can be shared with a family GP antenatally, who can liaise with the hospital during this time. However, in the case of sharing with standard care, there is no way of knowing who will be attending you during your birth.
The Case for Continuity- What the Evidence Says
Continuity of care during pregnancy, birth and postpartum, with a known midwife, has long been considered to be the “gold standard” of care.

Continuity of Care with a midwife has been shown to:
- Be safe and cost-effective, with women of all risk levels, compared to standard care (Tracey et al, 2013)
- Reduce the likelihood of Cesarean section, instrumental birth and episiotomy in low-risk women, compared with other models of care (Sandall et al, 2024).
- Increase the likelihood of spontaneous vaginal birth in low-risk women (Sandall et al, 2024)
- Result in better outcomes for women planning a VBAC (vaginal birth after caesarean) (Keedle & Schmeid et al, 2020)
- Result in a more positive and satisfying birth experience (Sandall et al, 2024)
- Provide many more hours of direct, postnatal care for women. In my experience with a PPM I received over 13 hours of time with my midwife postnatally, as opposed to the average of 3-3.5 hours of direct care received in standard models (Schmied et al, 2024).
Further to that, one of the recommendations of the NSW Legislative Council’s Inquiry into Birth Trauma (2024) was that all women should have access to continuity of carer models in order to reduce instances of preventable birth trauma.
…What about private OBs?
So, does the research say that continuity with a known obstetrician results in similarly improved outcomes?
In short: no, it doesn’t.
We see a much higher rate of medical intervention for women who birth in private hospitals (continuity with an OB) compared with public hospitals (fragmented care) (Dahlen et al, 2014). In fact, the 2024 Australian Mother and Babies report stated that only 35% of women who gave birth in a private hospital had a non-instrumental vaginal birth, compared with 52% in the public hospital system.
And, according to Dahlen (2024), the increased intervention in private hospitals did not correlate with improved outcomes for babies, and women actually had poorer outcomes across a range of clinical criteria.
And yet, private OBs remain such a popular choice.
Here in Perth, Western Australia, a fairly large percentage of women choose a private OB, not because they are ill or have complicated pregnancies, but simply because they want the “best” care. That was me.
This belief that an OB always gives the most appropriate care is not based on the evidence, but actually based on our birthing culture. The dominant narrative in our society is that pregnancy is a pathological condition. That birth is a dangerous, medical event, which needs to be managed with gadgets and medicine.
Through this lens, it makes sense that women would opt for a doctor, particularly one who is known to them. But in reality, it is not the safest and best choice for all women, not according to the information we have.
It certainly was not the best choice for me.
I believe that even if I needed obstetric care for a complex pregnancy, it would have served me better to have continuity of care with a midwife who could consult with an OB at her affiliated hospital. That would have given the best of both worlds.
The Birth Experience Study (BESt)
Curious about the experiences of women in the Birth space, Professor Hannah Dahlen and Dr Hazel Keedle embarked on a massive study called the Birth Experience Study. One of the papers that they have produced, led by Helen Pelak, is A content analysis of women’s experiences of different models of maternity care: the Birth Experience Study (BESt).
If you are curious about the strengths and limitations of different care models, check out their findings. (Spoiler: Private Midwifery had the highest strengths and the lowest limitations!)
Apples and Oranges and the Biggest Decision
Midwives and OBs operate so very differently because they have completely different job descriptions. Both have a specialised skill set, and both are crucial to our maternity care system. However, they may not be equally good options for you, an individual, in your antenatal, birth and postpartum care.

The most impactful decisions you make in pregnancy are where you birth and who you choose to support you.
If you have the luxury of choice- and sadly, it is a luxury- choosing a provider whose philosophy aligns with your own will increase the likelihood that you will have a positive and satisfying birth experience.
And, according to the best research we have, choosing continuity of care with a known midwife will put you in the best possible position for a positive birth and postnatal journey, no matter who you are.
References
Dahlen H.G., Tracy S., Tracy M., et a (2014) Rates of obstetric intervention and associated perinatal mortality and morbidity among low-risk women giving birth in private and public hospitals in NSW (2000–2008): a linked data population-based cohort study. BMJ Open 2014, 4, e004551. doi: 10.1136/bmjopen-2013-004551
Jobs and Skills Australia, Australian Government Website. https://www.jobsandskills.gov.au/data/occupation-and-industry-profiles/occupations
Keedle, H., Peters, L., Schmied, V. et al. (2020) Women’s experiences of planning a vaginal birth after caesarean in different models of maternity care in Australia. BMC Pregnancy Childbirth, 20, 381. https://doi.org/10.1186/s12884-020-03075-8
Method of Birth, Australia’s Mothers and Babies 2024. https://www.aihw.gov.au/reports/mothers-babies/australias-mothers-babies/contents/labour-and-birth/method-of-birth
Pelak, H., Dahlen, H.G. & Keedle, H. A content analysis of women’s experiences of different models of maternity care: the Birth Experience Study (BESt). BMC Pregnancy Childbirth 23, 864 (2023). https://doi.org/10.1186/s12884-023-06130-2
Sandall J., Fernandez Turienzo C., Devane D., Soltani H., Gillespie P., Gates S., Jones L.V., Shennan A.H., Rayment-Jones H. (2024). Midwife continuity of care models versus other models of care for childbearing women. Cochrane Database of Systematic Reviews 2024, 4, DOI: 10.1002/14651858.CD004667.pub6.
Schmied, V., Myors, K., Burns, E. et al.(2024) A mixed methods study of the postnatal care journey from birth to discharge in a maternity service in New South Wales, Australia. BMC Health Serv Res 24, 1530. https://doi.org/10.1186/s12913-024-11995-w
Tracy, S.K. et al. (2013). Caseload midwifery care versus standard maternity care for women of any risk: M@NGO, a randomised controlled trial. The Lancet, 382, 9906, 1723 – 1732. https://pubmed.ncbi.nlm.nih.gov/24050808/
Follow Me & Subscribe
A WordPress.com site.

Leave a reply to Midwifery Continuity of Care: Solid Gold – Perth Birth Nerd Cancel reply